Maintaining essential gum health is pivotal for both oral and systemic wellbeing. Recognizing the early signs of gum disease, such as persistent bad breath or gum bleeding, is indispensable. Individuals in Atlanta, GA should consider consulting a periodontist, especially if they possess risk factors like smoking or diabetes. Seeking the best periodontal treatment in Atlanta, GA can prevent irreversible damage, preserve natural teeth, and ensure comprehensive care tailored to each patient’s needs. Understanding when to seek specialized care is paramount to safeguarding oral health.
Signs of Gum Disease You Shouldn’t Ignore
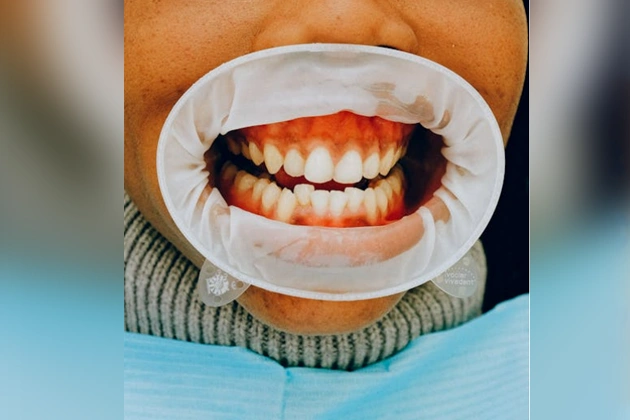
How can one recognize the early indicators of gum disease that require attention? Initial signs include changes in gum inflammation severity and gum bleeding concerns. Mild gum inflammation may become evident through redness and swelling, while more severe cases can lead to gum recession. Regular bleeding during brushing or flossing is another concerning symptom that suggests compromised gum health. These manifestations often indicate underlying issues that necessitate further examination. Observing the progression from minor discomfort to persistent symptoms can help in determining the necessity for professional consultation. Identifying these signs early is integral to preventing more severe periodontal conditions. In this manner, individuals are advised to monitor these symptoms closely and seek evaluation from a periodontist if changes in gum health persist or worsen.
Persistent Bad Breath and Its Connection to Gum Health
Persistent bad breath, medically known as halitosis, is often an overlooked indication of gum health issues. It arises due to inadequate oral hygiene practices and underlying gum problems. Four key factors contribute to this condition:
- Bacterial Buildup: Poor oral hygiene practices lead to bacterial accumulation on the tongue and gums, producing volatile sulfur compounds.
- Gum Inflammation: Chronic gum inflammation results in tissue breakdown and bacterial growth, exacerbating halitosis.
- Plaque Formation: Ineffective brushing and flossing allow plaque to harden into tartar, facilitating bacterial proliferation.
- Periodontal Disease: Advanced gum disease not only damages tissues but also perpetuates bad breath.
Effective gum inflammation management and rigorous oral hygiene practices are crucial in addressing halitosis and maintaining ideal gum health.
The Role of Genetics in Periodontal Health
Genetics plays a significant role in periodontal health, influencing an individual’s susceptibility to gum disease and overall oral health outcomes. Hereditary factors contribute to the variation in the immune responses and inflammatory processes related to periodontal diseases. Individuals with a genetic predisposition may exhibit an increased risk of developing conditions such as gingivitis and periodontitis, despite maintaining good oral hygiene practices. Various studies have identified specific gene polymorphisms associated with increased vulnerability to periodontal destruction. These genetic markers can modulate host responses to bacterial plaque, influencing the severity and progression of gum disease. Understanding these hereditary factors enables dental professionals to tailor preventive and therapeutic strategies, emphasizing the importance of genetic screening in extensive periodontal evaluations for patients with family histories of gum issues.
Recognizing the Symptoms of Gingivitis
Gingivitis, a common and mild form of periodontal disease, can often be identified by several early warning signs that necessitate prompt attention. Changes in gum color, such as redness or darkening, along with persistent bad breath, are key indicators that should not be overlooked. Early detection of these symptoms is critical in preventing the progression to more severe periodontal conditions.
Early Warning Signs
When individuals notice subtle changes in their oral health, it might indicate the early stages of gingivitis. Early detection is critical to prevent progression into more severe periodontal disease. Key indicators include:
- Gum Inflammation: Swelling and redness around the gums often signify an immune response to plaque buildup, necessitating immediate attention.
- Receding Gum Line: Observing a noticeable shift in the gum line can expose tooth roots, increasing sensitivity and risk of decay.
- Bleeding Gums: Bleeding during brushing or flossing is a common early warning sign, suggesting weakened gum tissue integrity.
- Persistent Bad Breath: Also known as halitosis, it can result from bacteria accumulation in the mouth, indicating poor gum health.
Recognizing these signs early can prompt timely intervention by a dental professional.
Gum Color Changes
In addition to inflammation and bleeding, changes in gum color serve as a significant indicator of gingivitis. Healthy gums typically exhibit a consistent pink hue. However, the presence of discolored gums or gum pigmentation changes may suggest underlying periodontal issues. These alterations can manifest as red, purple, or even white patches on the gum tissue. Such discoloration results from increased blood flow or the breakdown of gum tissues due to bacterial activity, signaling the onset of gingivitis. Early detection of these symptoms is essential, as they often precede more severe periodontal diseases. Consulting a periodontist in Atlanta, GA, upon noticing these changes is advisable to obtain a professional assessment and prevent further gum deterioration. Recognizing these signs aids in timely intervention and effective treatment.
Persistent Bad Breath
How often does one consider that persistent bad breath might be more than just an oral hygiene issue? Often overlooked, halitosis can be an early indicator of gingivitis. This condition arises from poor oral hygiene and improper brushing technique, leading to plaque buildup and inflammation. Identifying the symptoms early is essential for preventing progression to periodontal disease.
Consider the following factors:
- Consistency: Persistent bad breath that does not improve with regular brushing and flossing.
- Technique: Improper brushing technique may leave behind food particles, fostering bacterial growth.
- Gum Condition: Swollen or bleeding gums may accompany bad breath, indicating underlying issues.
- Professional Evaluation: Consulting a periodontist can provide a thorough assessment and tailored treatment plan.
Recognizing these signs enables timely intervention.
Advanced Periodontitis: When to Seek Immediate Care
Why does advanced periodontitis necessitate immediate care? This severe gum disease stage gravely threatens oral health, characterized by severe tooth mobility and advanced bone loss. As periodontitis progresses, bacteria penetrate deeper into the gums, causing inflammation and destruction of supportive tissues and bone. The resulting advanced bone loss compromises the stability of teeth, leading to severe tooth mobility and potential tooth loss if untreated. Immediate care from a periodontist is essential to halt disease progression and mitigate further damage. Intervention may involve surgical procedures, such as flap surgery or bone grafting, to restore gum and bone health. Early detection and prompt treatment by a periodontist in Atlanta, GA can prevent irreversible damage and maintain oral functionality, emphasizing the importance of timely professional intervention.
Impact of Smoking on Your Gums
Addressing advanced periodontitis highlights the critical nature of maintaining gum health, a task markedly hindered by smoking. Smoking introduces numerous challenges to oral health, primarily through:
- Increased Plaque Buildup: Smoking fosters a conducive environment for plaque accumulation, complicating oral hygiene efforts and exacerbating periodontal disease.
- Accelerated Gum Recession: Chemicals in tobacco products contribute to the deterioration of gum tissue, leading to faster gum recession and exposing tooth roots.
- Reduced Blood Flow: Nicotine constricts blood vessels, diminishing essential blood supply to the gums, which impairs healing and defense against infections.
- Altered Immune Response: The immune system’s effectiveness is compromised, increasing susceptibility to infections and hindering recovery from gum disease.
These factors emphasize the necessity for smokers to seek regular periodontal evaluations to mitigate adverse effects.
Gum Health During Pregnancy: What to Watch For
During pregnancy, hormonal changes can increase the risk of developing pregnancy gingivitis, characterized by red, swollen, and bleeding gums. It is vital for expectant mothers to schedule regular dental checkups to monitor and manage gum health effectively. Prompt attention to these symptoms can prevent more severe periodontal issues and support overall maternal and fetal well-being.
Pregnancy Gingivitis Symptoms
Pregnancy can bring about numerous changes in a woman’s body, and one such area affected is oral health, specifically the gums. Hormonal changes during pregnancy can exacerbate the body’s response to plaque accumulation, leading to pregnancy gingivitis. Recognizing the symptoms is vital for maintaining gum health.
- Redness and Swelling: Gums may appear more inflamed and exhibit noticeable redness.
- Bleeding Gums: Increased bleeding, especially during brushing or flossing, is common.
- Tenderness: Gums may become sensitive or painful to touch.
- Bad Breath: Persistent halitosis can be a sign of underlying gum issues.
These symptoms highlight the importance of maintaining oral hygiene and monitoring changes during pregnancy. Pregnant individuals should consult healthcare providers if these symptoms persist.
Importance of Regular Checkups
Regular dental checkups are essential for monitoring gum health, especially during pregnancy when hormonal changes can markedly impact oral conditions. These physiological shifts can lead to increased susceptibility to gingivitis and other periodontal issues. Ensuring timely professional cleanings helps in the removal of plaque and tartar that can exacerbate these conditions. Dental professionals can assess gum health and implement early intervention strategies to prevent progression into more severe periodontal disease. Regular visits enable the detection of subtle changes in gum tissue that may not be immediately noticeable to the untrained eye. Ultimately, consistent monitoring and maintenance through routine checkups are indispensable in preserving oral health during pregnancy, safeguarding both maternal and fetal well-being from potential systemic health implications.
The Link Between Diabetes and Periodontal Disease
A significant connection exists between diabetes and periodontal disease, underscoring the importance of understanding this relationship for effective gum health management. Elevated blood glucose levels and increased insulin resistance are pivotal factors linking these conditions. Diabetic patients may face a higher risk of periodontal disease due to:
- Inflammatory Response: Diabetes can exacerbate inflammation, worsening gum issues.
- Vascular Changes: Impaired blood flow in diabetics hinders gum healing processes.
- Immune Dysfunction: Diabetes can weaken the body’s defense against bacterial infections in gums.
- Oral Microbiome Alteration: Elevated glucose can alter the oral environment, favoring harmful bacteria.
Understanding these interactions provides a foundation for targeted periodontal care, essential for maintaining oral health in diabetic individuals.
Benefits of Regular Periodontal Check-Ups
Given the well-documented connection between diabetes and periodontal disease, consistent periodontal check-ups emerge as a strategic approach to mitigating gum health issues, particularly for those at increased risk. Regular periodontal checkup frequency allows for early detection and management of periodontal conditions, preventing progression. Professional cleaning, a key component of these check-ups, effectively removes calculus and plaque, reducing inflammation and promoting oral health.
The benefits of professional cleaning extend to minimizing bacteria that can exacerbate systemic conditions, including diabetes. Furthermore, frequent assessments enable personalized care plans, optimizing treatment outcomes. For individuals with a predisposition to periodontal disease, scheduled visits to a periodontist in Atlanta, GA, are essential for maintaining gum health and preventing complex dental interventions. Consistent check-ups guarantee proactive management of periodontal health.
Frequently Asked Questions
How Does Stress Affect Gum Health?
Stress affects gum health by triggering stress induced inflammation, compromising the body’s ability to combat bacteria due to a stress related immune response. This can exacerbate periodontal disease, leading to gum recession and potential tooth loss.
Can Diet Influence Periodontal Disease?
Diet can considerably influence periodontal disease. Increased dietary fiber intake may reduce inflammation, while nutritional deficiencies, particularly in vitamins C and D, can exacerbate gum disease by impairing the body’s ability to maintain healthy periodontal tissue.
Is It Necessary to Replace Missing Teeth for Gum Health?
Replacing missing teeth is essential for maintaining gum health. Missing teeth can lead to bone loss, shifting of adjacent teeth, and increased susceptibility to periodontal disease, highlighting the importance of replacing missing teeth for overall oral health stability.
Are There Natural Remedies for Improving Gum Health?
Natural remedies for improving gum health include herbal supplements like chamomile and green tea, known for their anti-inflammatory properties. Oil pulling with coconut oil may also reduce plaque and bacteria, promoting healthier gums.
How Does Hormonal Change Affect Gums?
Hormonal fluctuations can markedly impact gum health, leading to gingival inflammation. Changes in hormone levels during puberty, pregnancy, menstruation, or menopause increase blood flow to the gums, making them more sensitive, swollen, and prone to bleeding.