Quick Answer
Testosterone replacement therapy can help men with clinically low levels regain energy, stabilize mood, and improve physical well-being. As it naturally declines with age or due to medical conditions, symptoms like fatigue, irritability, reduced muscle mass, and low motivation may emerge. Restoring hormone balance through medically supervised therapy often leads to better sleep, sharper focus, increased strength, and enhanced emotional resilience – supporting long-term health and quality of life.
Introduction
Testosterone plays a central role in men’s physical and mental health far beyond its association with virility. It influences everything from muscle maintenance and bone density to motivation, concentration, and emotional regulation. Yet hormone levels typically begin to decline after age 30, sometimes more sharply due to chronic illness, obesity, or genetic factors.
When this drop is significant, it can trigger a cascade of symptoms that affect daily life. Leo for Men’s testosterone replacement therapy provides a comprehensive approach focused on natural hormone optimization. Understanding what TRT is and how it impacts physical and emotional health paves the way for informed decisions about maintaining vitality and well-being throughout life.
What Is TRT? Understanding the Science and Scope
Testosterone replacement therapy (TRT) is a clinically guided intervention for men with confirmed low testosterone levels – also known as hypogonadism. Far from a lifestyle trend, TRT addresses a measurable hormonal imbalance that can significantly affect physical, mental, and metabolic health. It is used only after thorough evaluation, including blood work and symptom assessment, to confirm a true deficiency.
The Biological Role of Testosterone
This hormone is the primary androgen in men, responsible for:
- Development of male characteristics during puberty
- Maintenance of muscle mass and bone density
- Regulation of red blood cell production
- Support of libido, mood stability, and cognitive function
After age 30, levels typically decline by about 1% per year. While this is normal, a steeper drop – often accelerated by obesity, chronic illness, or environmental factors – can lead to disruptive symptoms that impact daily life.
How TRT Works in Clinical Practice
TRT aims to restore testosterone to a normal, healthy range – not to exceed it. Treatment begins with diagnostic testing, followed by a personalized delivery method. Common options include:
- Topical gels: Applied daily to clean skin, absorbed through the epidermis
- Intramuscular injections: Administered every 1–2 weeks for steady hormone release
- Subcutaneous pellets: Implanted under the skin and release testosterone gradually over months
Each method has distinct pharmacokinetics, and the choice depends on patient preference, lifestyle, and clinical response.
TRT vs. Anabolic Steroids: A Critical Distinction
It’s important to differentiate medically supervised TRT from unsupervised anabolic steroid use:
- TRT uses bioidentical testosterone at doses calibrated to achieve physiological levels
- Anabolic steroids often involve supraphysiological doses with non-medical goals, carrying higher risks
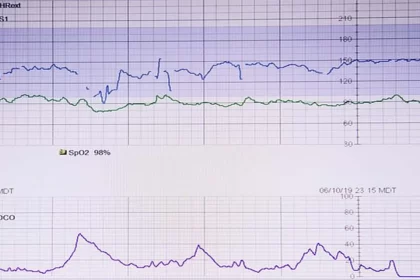
Under proper care, TRT is monitored through regular blood tests, symptom tracking, and checks for potential side effects like elevated hematocrit or changes in sleep apnea.
How Does Testosterone Affect Mood and Physical Health
Hormone interacts with multiple systems in the body, making their influence both widespread and subtle. Its decline rarely shows up as one dramatic change but rather as a gradual shift in how men feel, think, and function.
Mood Stability and Emotional Resilience
Low testosterone is often linked to increased irritability, low mood, or a sense of emotional flatness. The hormone modulates key neurotransmitters like serotonin and dopamine, which help regulate stress response and motivation. When levels fall, men may notice they’re less patient, more withdrawn, or struggle to find enjoyment in activities they once valued.
Sustained Energy and Mental Clarity
Fatigue that isn’t resolved by rest can be a red flag. Testosterone supports mitochondrial function – the energy factories in cells – particularly in muscle and brain tissue. Men with low levels often report brain fog, difficulty concentrating, or a persistent lack of drive. Restoring balance may improve cognitive sharpness and the stamina needed for work, hobbies, or family life.
Body Composition and Strength
Testosterone drives muscle protein synthesis and helps maintain lean mass. As levels drop, fat accumulation – especially around the abdomen – tends to increase, even with consistent exercise. Simultaneously, bone mineral density may weaken, raising fracture risk. Therapy can help reverse these trends, supporting mobility and metabolic health over time.
Sleep Quality and Recovery
The relationship between sleep and testosterone is bidirectional. Poor sleep suppresses hormone production, while hypogonadism can disrupt deep sleep cycles. Addressing a deficiency often leads to more restful nights, which in turn supports immune function, mood, and daytime alertness.
Recognizing Symptoms of Low Testosterone
Not every change in energy or mood signals a hormone issue. But when several symptoms cluster together – especially in men over 40 – it may warrant medical evaluation.
Common physical signs include:
- Unexplained fatigue despite adequate rest
- Loss of muscle tone or reduced exercise tolerance
- Increased abdominal fat or difficulty managing weight
- Declining libido or changes in sexual function
- Thinning body or facial hair
Emotional and cognitive indicators may involve:
- Persistent low mood or lack of motivation
- Heightened anxiety or emotional reactivity
- Trouble focusing or recalling details
- Reduced confidence or sense of purpose
Diagnosis typically begins with a morning blood test to measure total and free testosterone, alongside a review of medical history. Provincial health guidelines emphasize ruling out other causes – such as thyroid dysfunction or depression – before considering hormone therapy.
Delivery Methods for Testosterone Replacement
Several FDA-approved (and Health Canada-recognized) options exist, each with distinct advantages. The right choice depends on lifestyle, symptom severity, and personal preference.
| Method | How It Works | Duration | Key Benefits | Considerations |
| Injections | Intramuscular or subcutaneous | 1–3 weeks | Cost-effective; rapid results | Hormone fluctuations; clinic visits |
| Topical gels | Applied to clean, dry skin | Daily | Steady absorption; non-invasive | Risk of skin transfer; daily routine |
| Patches | Adhered to abdomen, back, or arm | 24 hours | Consistent delivery | Skin irritation; visibility |
| Subcutaneous pellets | Implanted under skin | 3–6 months | Long-lasting; no daily action needed | Minor procedure; potential migration |
Oral formulations remain limited in Canada due to liver safety concerns, though newer buccal (gum-absorbed) options are occasionally used under specialist supervision.
Working with a knowledgeable provider ensures proper dosing and ongoing monitoring of hematocrit, prostate health, and lipid levels – key steps in maintaining safety during long-term therapy. Testosterone therapy for men is most effective when paired with regular follow-ups, lifestyle support, and realistic expectations.
Final Takeaways: TRT as a Path to Balanced Well-Being
Testosterone replacement therapy offers more than just a boost in physical performance – it supports emotional stability, sustained energy, and long-term metabolic health in men with clinically low levels. For those experiencing persistent fatigue, low drive, or mood shifts, evaluating whether such therapy is appropriate may be a vital step toward reclaiming daily well-being.